Home | Specialties | Occupational Therapy | Neural Mobilization
Neural Mobilization
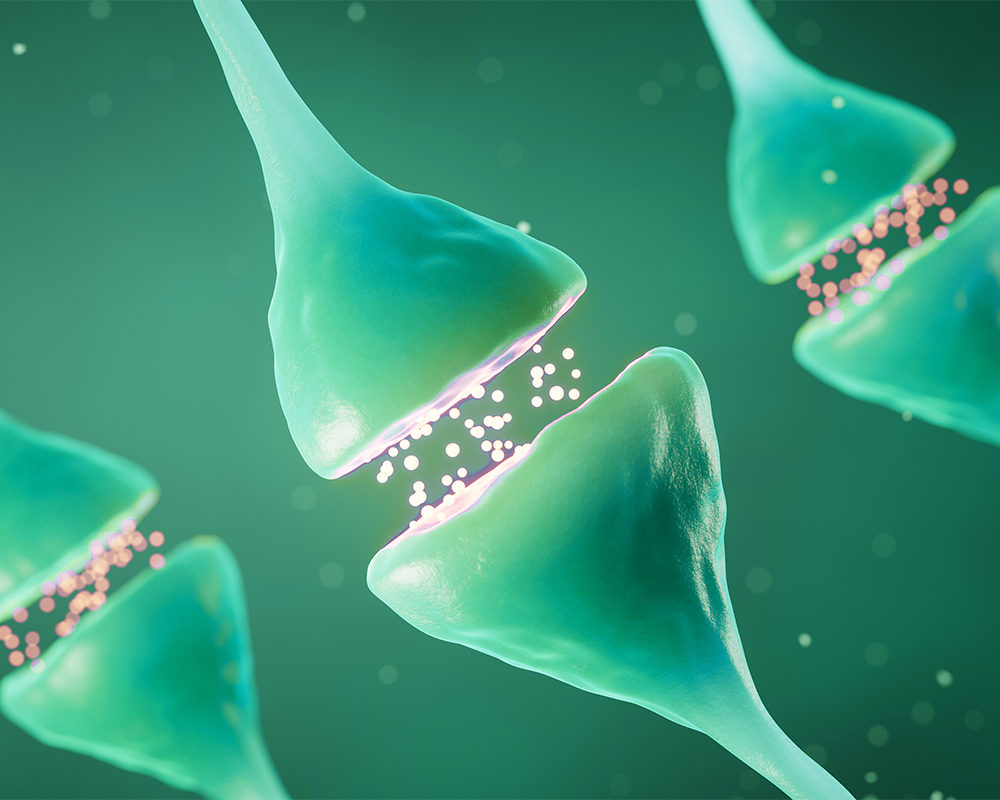
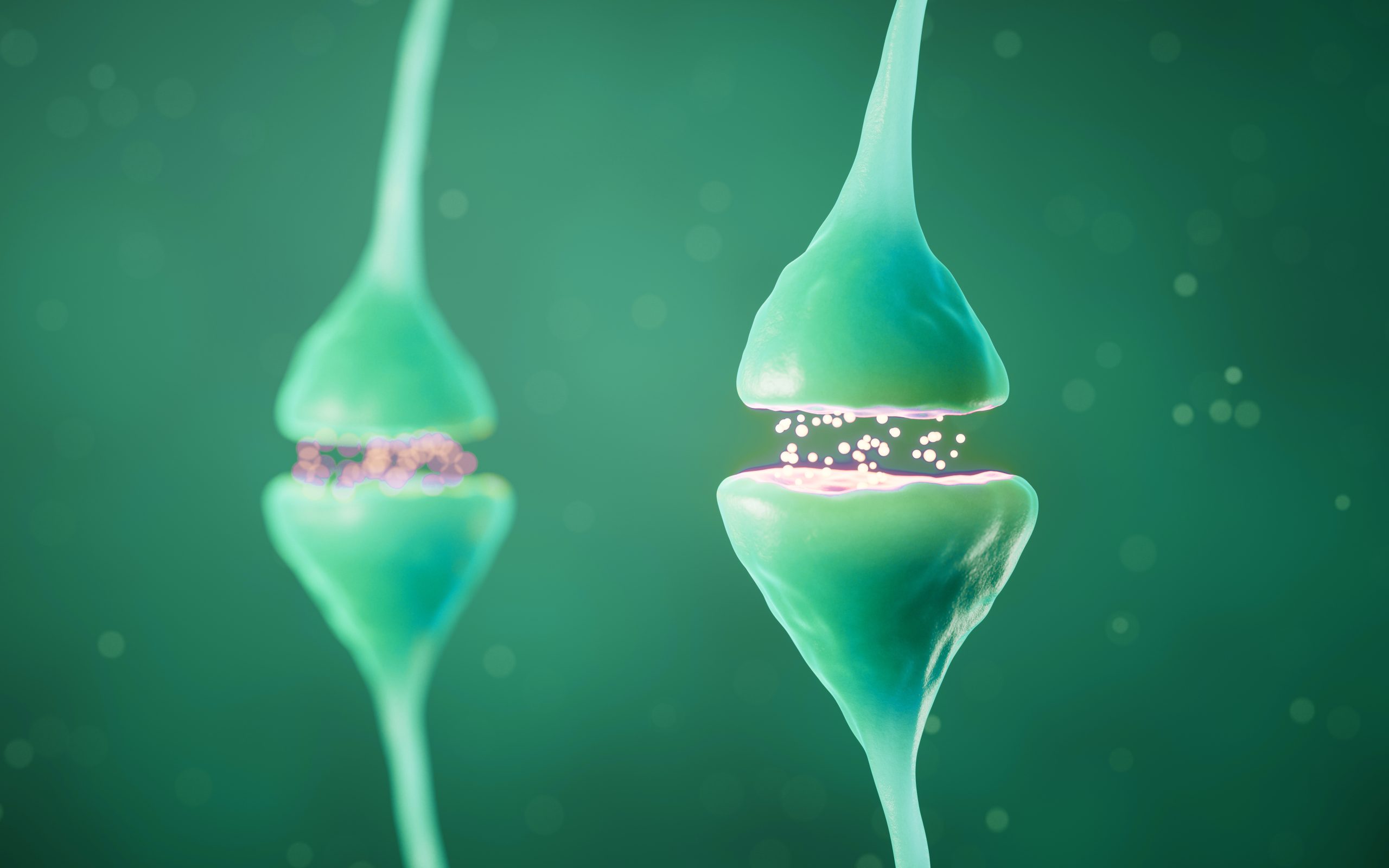
Neural mobilization, also known as neural gliding or neural tension techniques, is a therapeutic approach used in occupational therapy and physical therapy to address conditions involving nerve-related symptoms. It focuses on improving the mobility and flexibility of neural structures, such as nerves, nerve roots, and the spinal cord, to alleviate pain, reduce nerve irritation, and restore normal nerve function.
Why Might You Need Neural Mobilization?
Neural Mobilization may be recommended if you experience:
- Nerve Pain: Chronic or acute pain associated with nerve compression or irritation.
- Reduced Mobility: Limited range of motion due to nerve restrictions.
- Post-Surgical Recovery: Recovery from surgeries that may have impacted nerve function.
- Chronic Conditions: Conditions such as carpal tunnel syndrome, sciatica, or other nerve entrapment syndromes.
- Injury Rehabilitation: Rehabilitation from injuries that have caused nerve damage or impairment.
What Are the Steps in a Neural Mobilization Procedure?
Pre-Treatment Preparation
- Medical Evaluation: Comprehensive review of your medical history, symptoms, and previous treatments.
- Physical Examination: Assessment of nerve function, range of motion, and areas of pain or restriction.
- Diagnostic Tests: Imaging studies or nerve conduction tests may be performed to identify the specific areas of nerve restriction.
During the Treatment
- Patient Positioning: You will be comfortably positioned to allow easy access to the affected area.
- Manual Techniques: The therapist uses hands-on techniques to gently mobilize the nerve, including stretching and gliding movements.
- Guided Exercises: Specific exercises are performed to enhance nerve mobility and reduce tension.
- Patient Education: Instruction on how to perform exercises at home to maintain improvements and prevent recurrence.
Post-Treatment Care
- Observation: Monitoring of your response to the treatment and adjustments as needed.
- Pain Management: Techniques and advice on managing any discomfort following the treatment.
- Activity Guidelines: Recommendations for activities to avoid and those to incorporate into your daily routine to support recovery.
- Follow-Up Sessions: Scheduled therapy sessions to continue progress and ensure lasting benefits.
Recovery and Rehabilitation
Post-Treatment Care
- Pain Monitoring: Keeping track of pain levels and any changes in symptoms to guide further treatment.
- Home Exercises: Continued practice of prescribed exercises to maintain nerve mobility and prevent stiffness.
- Progress Evaluation: Regular assessments to monitor improvements in function and mobility.
Potential Complications
While Neural Mobilization is generally safe, potential complications can include:
- Initial Discomfort: Mild discomfort or soreness following the treatment, which typically resolves quickly.
- Temporary Exacerbation: Temporary increase in symptoms as the nerves adjust to new mobility.
- Individual Variability: Differences in individual response to treatment, requiring personalized adjustments.
Benefits of Neural Mobilization in Occupational Therapy
- Pain Relief: Reduction in nerve-related pain and discomfort.
- Improved Mobility: Enhanced range of motion and flexibility in the affected areas.
- Functional Restoration: Restoration of normal nerve function, facilitating daily activities and overall hand use.
- Enhanced Quality of Life: Improved overall well-being and ability to participate in work and leisure activities without nerve pain or restrictions.
