Home | Specialties | Physical Therapy | Post-Operative Orthopedic Care
Post-Operative Orthopedic Care
Post-operative orthopedic care in physical therapy refers to the specialized rehabilitation and treatment provided to individuals after orthopedic surgery. It aims to facilitate the recovery process, restore optimal function, and promote successful outcomes following orthopedic procedures.

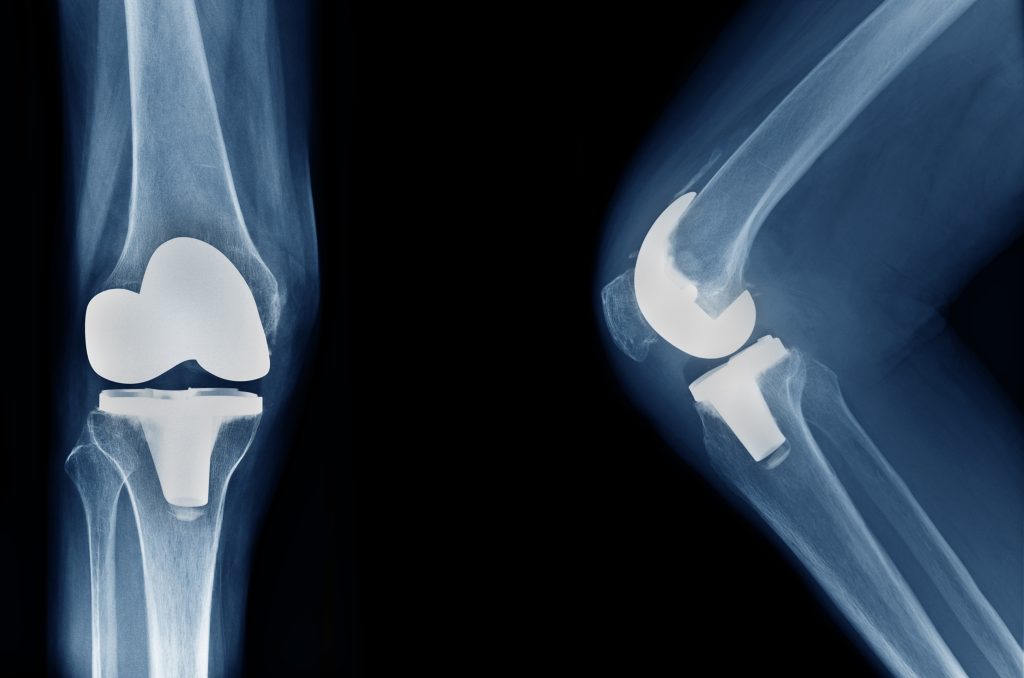
The physical therapy process for post-operative orthopedic care related to total joint replacement typically involves several stages:
Pain Management:
Managing pain is an important aspect of post-operative care. The physical therapist may use various techniques such as ice or heat therapy, electrical stimulation, or manual techniques to help alleviate pain and discomfort.
Early Mobilization:
The physical therapist will guide the patient in performing gentle exercises and movements to promote early mobilization of the joint. This helps prevent stiffness and promotes blood circulation for healing.
Range of Motion Exercises:
The physical therapist will guide the patient through a series of range of motion exercises to gradually increase the mobility of the replaced joint. These exercises aim to improve flexibility, reduce stiffness, and restore normal joint movement.
Strengthening Exercises:
As the healing progresses, the physical therapist will introduce strengthening exercises to build muscle strength around the joint. These exercises target the specific muscles needed for joint stability and function.
Balance and Gait Training:
Restoring balance and normal gait (walking) patterns are important components of post-operative orthopedic care. The physical therapist will work with the patient on balance exercises and walking techniques to regain confidence and stability while walking.
Functional Activities:
The physical therapist will gradually incorporate functional activities into the therapy sessions. These activities simulate real-life tasks such as climbing stairs, getting in and out of a chair, or reaching for objects, with the goal of improving the patient’s ability to perform daily activities independently.
Education and Home Exercise Program:
The physical therapist will educate the patient on proper body mechanics, joint protection techniques, and strategies for managing activities at home. They will provide a personalized home exercise program consisting of exercises and activities to be performed independently to maintain progress and continue improving.
Throughout the physical therapy process, the therapist will closely monitor the patient’s progress, make adjustments to the treatment plan as needed, and provide ongoing support and guidance. The duration and frequency of physical therapy sessions will vary depending on individual factors such as the type of joint replacement, the patient’s overall health, and their specific goals for recovery. The ultimate aim is to optimize function, mobility, and quality of life following total joint replacement surgery.

Physical therapy plays a crucial role in the rehabilitation process following ACL reconstruction surgery. It aims to help patients regain strength, range of motion, stability, and function in the knee. Here are some ways in which physical therapy can assist in ACL reconstruction:
Early Post-Operative Phase:
Physical therapy begins shortly after surgery to manage pain, reduce swelling, and promote healing. The therapist may use techniques such as ice, elevation, and gentle manual therapy to facilitate recovery.
Range of Motion Exercises:
Physical therapists guide patients through exercises to restore full range of motion in the knee joint. This includes gentle stretching and bending exercises to prevent stiffness and increase flexibility.
Strengthening Exercises:
As the healing progresses, physical therapists prescribe specific exercises to strengthen the muscles surrounding the knee, including the quadriceps, hamstrings, and hip muscles. Strengthening these muscles provides stability and support to the knee joint.
Balance and Proprioception Training:
Physical therapy focuses on improving balance and proprioception, which is the body’s sense of position and movement. This training helps patients regain stability and coordination, reducing the risk of future injuries.
Functional Training:
Physical therapists work with patients to restore functional abilities necessary for daily activities and sports. This includes exercises that mimic the movements required for specific sports or activities, gradually reintroducing cutting, pivoting, jumping, and other dynamic movements.
Gait Training:
Proper walking and running mechanics are essential for optimal knee function. Physical therapists help patients develop a proper gait pattern and stride length to ensure a smooth and efficient movement pattern.
Sports-Specific Rehabilitation:
For athletes returning to sports, physical therapy focuses on sport-specific activities and drills to prepare them for a safe and successful return to their chosen sport. This may involve agility exercises, sport-specific movement patterns, and gradually increasing intensity and impact.
Education and Home Exercise Program:
Physical therapists provide education on post-operative care, activity modifications, and strategies to prevent re-injury. They also create a personalized home exercise program to maintain progress and continue strengthening outside of therapy sessions.
The duration and frequency of physical therapy sessions will vary depending on individual factors such as the patient’s progress, surgical technique, and specific goals. Physical therapy is a critical component of ACL reconstruction recovery, helping patients regain strength, function, and confidence in their knee for a successful return to an active lifestyle.

Physical therapy plays a crucial role in the rehabilitation process following a meniscus repair. Here are some ways in which physical therapy can help:
Reduce Pain and Swelling:
After a meniscus repair, physical therapy can help manage pain and reduce swelling through techniques such as ice or cold therapy, electrical stimulation, or manual therapy. These interventions can help alleviate discomfort and promote the healing process.
Restore Range of Motion:
Meniscus injuries and surgeries can result in limited range of motion in the knee. Physical therapy includes exercises and stretching techniques that aim to restore normal range of motion, allowing you to regain full mobility and function in your knee joint.
Strengthen the Knee and Surrounding Muscles:
Physical therapists will design a customized exercise program to strengthen the muscles around the knee, including the quadriceps, hamstrings, and calf muscles. Strengthening these muscles helps provide stability and support to the knee joint, reducing the risk of further injury and improving overall function.
Improve Balance and Stability:
Meniscus injuries can impact your balance and stability. Physical therapy will incorporate specific exercises and activities to enhance proprioception (awareness of joint position) and improve balance and stability. This is important for preventing falls and regaining confidence in your ability to move safely.
Gradually Resume Normal Activities:
Physical therapists will guide you through a progressive rehabilitation program to help you safely return to your normal activities. This may involve a gradual increase in weight-bearing exercises, functional movements, and sport-specific activities. They will closely monitor your progress and adjust the treatment plan accordingly.
Educate and Provide Home Exercise Program:
Physical therapists will educate you about your condition and teach you techniques and exercises that you can continue at home. This empowers you to take an active role in your recovery and optimize the long-term outcomes of your meniscus repair.
Prevent Future Injuries:
Physical therapy is not only focused on recovering from the current injury but also on preventing future injuries. Physical therapists will assess your movement patterns and provide guidance on proper body mechanics, biomechanics, and injury prevention strategies. This can help minimize the risk of re-injury or developing other knee-related problems.
By working closely with a physical therapist, following a structured rehabilitation program, and actively participating in your recovery, you can optimize the healing process, regain strength and mobility, and return to your daily activities and sports with confidence.

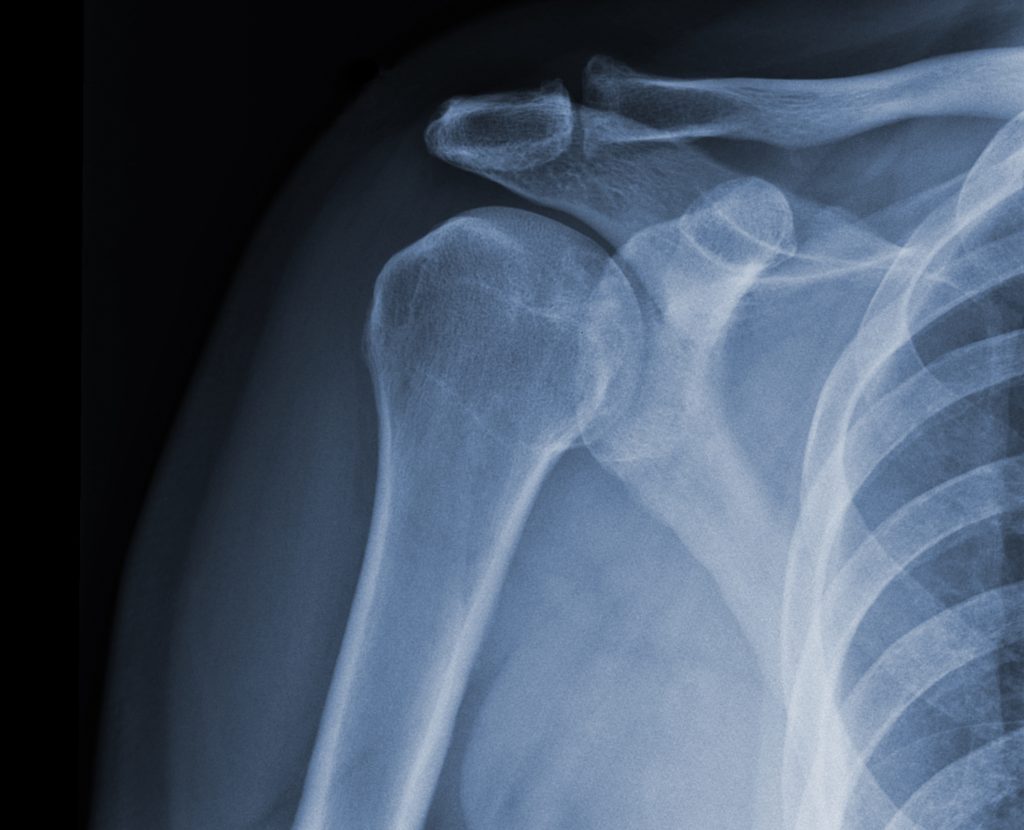
Physical therapy plays a crucial role in the rehabilitation process following a rotator cuff repair. Here are some ways in which physical therapy can help:
Manage Pain and Swelling:
After a rotator cuff repair surgery, physical therapy can help manage pain and reduce swelling through various modalities such as ice or cold therapy, electrical stimulation, or ultrasound. These techniques can help alleviate discomfort and promote healing.
Restore Range of Motion:
Rotator cuff injuries and surgeries can result in limited range of motion in the shoulder. Physical therapy includes gentle stretching exercises and techniques to gradually restore the normal range of motion in the shoulder joint. This helps prevent stiffness and improves functional movement.
Strengthen the Shoulder Muscles:
Physical therapists will design a customized exercise program to strengthen the muscles of the shoulder, including the rotator cuff muscles and surrounding muscles. Strengthening these muscles is important for providing stability and support to the shoulder joint, reducing the risk of re-injury, and improving overall shoulder function.
Improve Shoulder Stability and Posture:
Rotator cuff injuries can affect shoulder stability and posture. Physical therapy will include exercises and activities that focus on improving shoulder stability and posture. This helps restore proper alignment, balance, and coordination of the shoulder joint during daily activities and sports.
Enhance Shoulder Function:
Physical therapists will guide you through specific exercises and activities aimed at improving functional movements of the shoulder. This may include reaching overhead, lifting, pushing, and pulling activities. By gradually increasing the intensity and complexity of these movements, physical therapy helps you regain optimal shoulder function.
Educate and Provide Home Exercise Program:
Physical therapists will educate you about your condition, proper body mechanics, and strategies to prevent future injuries. They will also provide you with a personalized home exercise program to continue your rehabilitation independently. This empowers you to take an active role in your recovery and maintain the gains achieved during therapy sessions.
Gradual Return to Activities and Sports:
Physical therapists will work with you to develop a gradual return-to-activity plan based on your specific needs and goals. They will guide you through a progressive rehabilitation program, monitor your progress, and provide appropriate modifications to ensure a safe and successful return to your desired activities and sports.
By working closely with a physical therapist, following a structured rehabilitation program, and actively participating in your recovery, you can optimize the healing process, regain strength and function in your shoulder, and return to your daily activities and sports with confidence.

Physical therapy plays an important role in the rehabilitation process following a biceps repair surgery. Here are some ways in which physical therapy can help:
Pain and Swelling Management:
Physical therapy can help manage pain and reduce swelling after a biceps repair surgery. Therapists may use modalities such as ice or cold therapy, electrical stimulation, or ultrasound to alleviate pain and promote healing.
Restoring Range of Motion:
Following a biceps repair, the shoulder and elbow joints may experience limited range of motion. Physical therapists will guide you through specific exercises and stretching techniques to gradually restore the normal range of motion in these joints. This helps prevent stiffness and improves functional movements.
Strengthening the Biceps and Surrounding Muscles:
Physical therapy includes exercises targeting the biceps muscle and surrounding muscles to regain strength and stability. Strengthening these muscles is crucial for optimal function and preventing future injuries.
Improving Flexibility and Muscle Balance:
Physical therapists will work on improving flexibility in the shoulder, elbow, and surrounding muscles. They will address muscle imbalances that may have contributed to the biceps injury and design a personalized program to restore proper alignment and movement patterns.
Functional Training:
Physical therapy includes functional exercises and activities that simulate real-life movements. These exercises help you regain strength, coordination, and stability in the affected arm, allowing you to confidently perform daily activities and sports.
Educating on Proper Body Mechanics:
Physical therapists will educate you on proper body mechanics and movement techniques to prevent re-injury. They will provide guidance on lifting, carrying, and performing activities that may put stress on the biceps muscle, helping you avoid unnecessary strain.
Gradual Return to Activities:
Physical therapists will develop a gradual return-to-activity plan based on your specific needs and goals. They will monitor your progress, provide appropriate modifications, and guide you through a progressive rehabilitation program to ensure a safe and successful return to your desired activities and sports.
By working closely with a physical therapist and following a structured rehabilitation program, you can optimize the healing process, regain strength and function in your biceps, and confidently return to your daily activities and sports.
Physical therapy is an essential part of the rehabilitation process following shoulder arthroscopy. Here’s how physical therapy can help:
Pain and Swelling Management:
After shoulder arthroscopy, physical therapy can help manage pain and reduce swelling through modalities like ice or cold therapy, electrical stimulation, or ultrasound. These techniques can alleviate discomfort and promote healing.
Restoring Range of Motion:
Shoulder arthroscopy can result in limited range of motion in the shoulder joint. Physical therapists will guide you through gentle stretching exercises and techniques to gradually restore the normal range of motion in the shoulder. This helps prevent stiffness and improves functional movement.
Strengthening the Shoulder Muscles:
Physical therapy includes exercises targeting the muscles surrounding the shoulder joint. These exercises aim to strengthen the rotator cuff muscles, deltoids, and other muscles involved in shoulder stability and movement. Strengthening these muscles is important for restoring stability and improving overall shoulder function.
Improving Shoulder Stability and Posture:
Shoulder arthroscopy can affect shoulder stability and posture. Physical therapists will focus on exercises and activities that improve shoulder stability and promote proper alignment and posture. This helps restore optimal shoulder function and reduces the risk of re-injury.
Enhancing Functional Movement:
Physical therapy will include specific exercises and activities to improve the shoulder’s functional movements, such as reaching, lifting, and carrying. These activities are tailored to your individual needs and help you regain strength, coordination, and confidence in performing daily tasks and sports-related activities.
Education and Home Exercise Program:
Physical therapists will provide education on proper body mechanics, posture, and strategies to prevent future shoulder injuries. They will also design a personalized home exercise program to continue your rehabilitation independently, ensuring you can maintain the gains achieved during therapy sessions.
Gradual Return to Activities and Sports:
Physical therapists will work with you to develop a gradual return-to-activity plan based on your specific needs and goals. They will monitor your progress, provide appropriate modifications, and guide you through a progressive rehabilitation program to ensure a safe and successful return to your desired activities and sports.
By working closely with a physical therapist, following a structured rehabilitation program, and actively participating in your recovery, you can optimize the healing process, regain strength and function in your shoulder, and confidently return to your daily activities and sports.
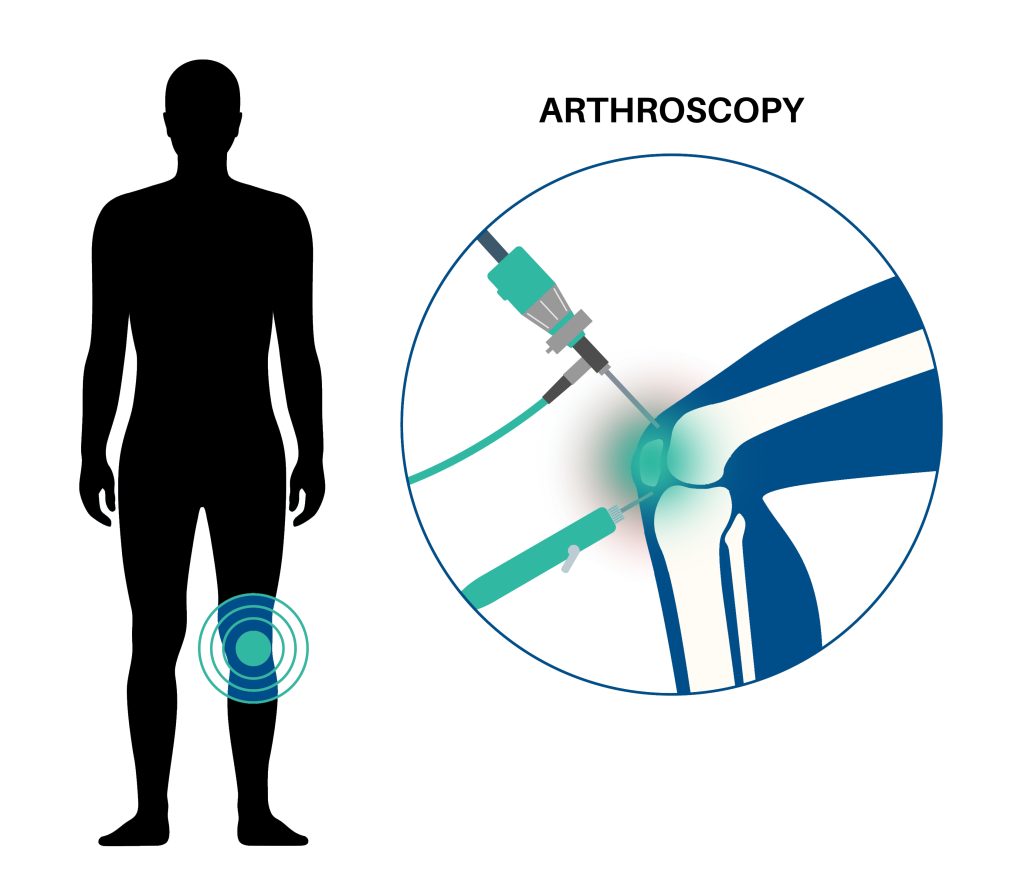
Physical therapy plays a crucial role in the rehabilitation process following knee arthroscopy. Here’s how physical therapy can help:
Pain and Swelling Management:
After knee arthroscopy, physical therapy can assist in managing pain and reducing swelling. Modalities such as ice or cold therapy, electrical stimulation, or ultrasound may be used to alleviate discomfort and promote healing.
Restoring Range of Motion:
Knee arthroscopy can result in decreased range of motion in the knee joint. Physical therapists will guide you through exercises and techniques to gradually restore the normal range of motion. This includes gentle stretching and joint mobilization to prevent stiffness and improve functional movement.
Strengthening the Knee Muscles:
Physical therapy includes exercises targeting the muscles surrounding the knee joint. Strengthening exercises help improve the stability of the knee and restore proper muscle balance. This may involve exercises for the quadriceps, hamstrings, calves, and hip muscles to enhance overall knee function.
Improving Balance and Proprioception:
Knee arthroscopy can affect balance and proprioception (awareness of joint position). Physical therapists will incorporate exercises and activities that challenge your balance and improve proprioception. These exercises can enhance joint stability and reduce the risk of falls and future injuries.
Enhancing Flexibility:
Physical therapy focuses on improving flexibility in the muscles surrounding the knee, such as the quadriceps and hamstrings. Stretching exercises are utilized to increase flexibility, promote proper joint alignment, and facilitate normal movement patterns.
Functional Training:
Physical therapists will incorporate functional exercises and activities into your rehabilitation program. These exercises simulate real-life movements and tasks, such as walking, climbing stairs, or getting up from a chair. Functional training helps you regain strength, coordination, and confidence in performing daily activities and sports-related movements.
Education and Home Exercise Program:
Physical therapists will provide education on proper body mechanics, joint protection, and strategies to prevent future knee injuries. They will also design a personalized home exercise program for you to continue your rehabilitation independently, ensuring that you can maintain the progress made during therapy sessions.
Gradual Return to Activities and Sports:
Physical therapists will develop a gradual return-to-activity plan tailored to your specific needs and goals. They will monitor your progress, provide appropriate modifications, and guide you through a progressive rehabilitation program to ensure a safe and successful return to your desired activities and sports.
By actively participating in physical therapy and following a structured rehabilitation program, you can optimize the healing process, regain strength and function in your knee, and confidently return to your daily activities and sports.

Physical therapy plays a vital role in the rehabilitation process following spinal fusion surgery. Here’s how physical therapy can help:
Pain Management:
After spinal fusion surgery, physical therapists can help manage pain through various modalities such as heat or cold therapy, electrical stimulation, or ultrasound. They may also teach you pain-relieving techniques and assistive devices to minimize discomfort during the healing process.
Restoring Range of Motion:
Spinal fusion surgery may result in a limited range of motion in the spine. Physical therapists will guide you through gentle exercises and techniques to gradually restore flexibility and mobility in the spine. These exercises focus on improving spinal alignment, reducing stiffness, and enhancing functional movement.
Strengthening the Core and Back Muscles:
Physical therapy includes exercises targeting the core and back muscles to provide stability and support to the spine. Strengthening these muscles can help compensate for the fused spinal segments, reduce stress on the surrounding structures, and improve overall posture and spinal function.
Improving Posture and Body Mechanics:
Physical therapists will work with you to improve your posture and body mechanics. They will teach you proper body alignment and movement patterns to reduce strain on the spine and promote optimal spinal health. This includes techniques for sitting, standing, lifting, and performing activities of daily living.
Enhancing Functional Mobility:
Physical therapy focuses on improving functional mobility and independence. Therapists will develop a customized program to address your specific needs, such as walking, balance training, and coordination exercises. These activities aim to improve your ability to perform daily tasks and regain independence.
Education and Lifestyle Modification:
Physical therapists provide education on spine health, ergonomics, and lifestyle modifications to help prevent future spinal issues. They may advise you on proper body mechanics, safe exercise techniques, and strategies to maintain a healthy spine in your daily activities and work environment.
Gradual Return to Activities:
Physical therapists will develop a gradual return-to-activity plan tailored to your specific needs and goals. They will monitor your progress, provide appropriate modifications, and guide you through a progressive rehabilitation program to ensure a safe and successful return to your desired activities and hobbies.
By actively participating in physical therapy and following a structured rehabilitation program, you can optimize the healing process, regain strength and mobility in your spine, and improve your overall function and quality of life following spinal fusion surgery.
