"Reclaim Your Independence with Skilled Manual Therapy!"
Skilled Manual Therapy
Skilled manual therapy in the context of occupational therapy refers to the use of hands-on techniques by occupational therapists to address physical impairments, promote functional abilities, and enhance participation in meaningful activities. Occupational therapists with advanced training and expertise utilize skilled manual therapy techniques as part of a comprehensive treatment approach.

Forms Of Care We Provide

The steps involved may vary depending on the specific technique being used and the individual’s condition:
Assessment:
The occupational therapist performs an assessment to evaluate the individual’s condition, identify areas of soft tissue dysfunction, and determine the appropriate technique for soft tissue mobilization. This assessment may include observation, palpation, range of motion testing, and gathering relevant medical history.
Positioning:
The therapist positions the individual in a comfortable and accessible position that allows for optimal access to the target soft tissues. This may involve sitting, lying down, or assuming a specific posture based on the area being treated.
Warm-up:
The therapist may use various methods to warm up the tissues before starting the manual therapy. This can include applying heat packs, using warm towels, or performing gentle exercises or movements to increase blood flow and relax the muscles.
Palpation:
The therapist palpates the target soft tissues to locate areas of tension, adhesions, or restrictions. This involves using their hands or fingers to feel for abnormal tissue texture, tightness, or knots within the muscles and surrounding soft tissues.
Application of Pressure:
The therapist applies controlled pressure to the target soft tissues using their hands, fingers, palms, or specialized tools. They may use gliding strokes, circular motions, or sustained pressure depending on the specific technique being employed.
Tissue Mobilization:
The therapist uses specific techniques to mobilize the soft tissues, such as kneading, rolling, or stretching the tissues. They apply varying amounts of pressure, direction, and speed based on the individual’s response and the intended therapeutic effect.
Communication and Feedback:
Throughout the session, the therapist maintains open communication with the individual to ensure their comfort and to gather feedback on the level of pressure, discomfort, or any sensations experienced. This helps guide the therapist in adjusting their techniques and ensuring the individual’s needs are met.
Treatment Progression:
The therapist progresses the treatment by systematically addressing different areas of soft tissue dysfunction or focusing on specific regions of concern. They may adjust their techniques based on the individual’s response and modify the pressure or direction of their movements as needed.
Home Program:
The therapist provides instructions and recommendations for self-care and home exercises to complement the manual therapy. This may include specific exercises, stretches, or self-massage techniques that the individual can perform between therapy sessions.
Progress Monitoring and Adjustment:
The therapist regularly assesses the individual’s progress, adjusts the treatment plan as needed, and provides ongoing support and guidance throughout the soft tissue mobilization process.
The steps involved may vary depending on the specific technique being used and the individual’s condition:
Assessment:
The occupational therapist performs an assessment to evaluate the individual’s condition, identify areas of myofascial dysfunction, and determine the appropriate technique for myofascial release. This assessment may include observation, palpation, range of motion testing, and gathering relevant medical history.
Positioning:
The therapist positions the individual in a comfortable and accessible position that allows for optimal access to the target myofascial tissues. This may involve sitting, lying down, or assuming a specific posture based on the area being treated.
Warm-up:
The therapist may use various methods to warm up the tissues before starting the manual therapy. This can include applying heat packs, using warm towels, or performing gentle exercises or movements to increase blood flow and relax the muscles.
Palpation:
The therapist palpates the target myofascial tissues to locate areas of tension, adhesions, or restrictions. This involves using their hands or fingers to feel for abnormal tissue texture, tightness, or knots within the muscles and surrounding fascia.
Engaging the Tissue:
The therapist applies pressure to the identified areas of myofascial dysfunction using their hands, fingers, palms, or specialized tools. They may use sustained pressure, gentle stretching, or a combination of techniques to engage and mobilize the tissues.
Direction and Duration:
The therapist applies pressure or stretches the myofascial tissues in a specific direction based on the identified restrictions and the intended therapeutic effect. They maintain the pressure for a sustained period, typically around 90 seconds, allowing the tissues to release and relax.
Communication and Feedback:
Throughout the session, the therapist maintains open communication with the individual to ensure their comfort and to gather feedback on the level of pressure, discomfort, or any sensations experienced. This helps guide the therapist in adjusting their techniques and ensuring the individual’s needs are met.
Treatment Progression:
The therapist progresses the treatment by systematically addressing different areas of myofascial dysfunction or focusing on specific regions of concern. They may adjust their techniques based on the individual’s response and modify the pressure, direction, or duration of their techniques as needed.
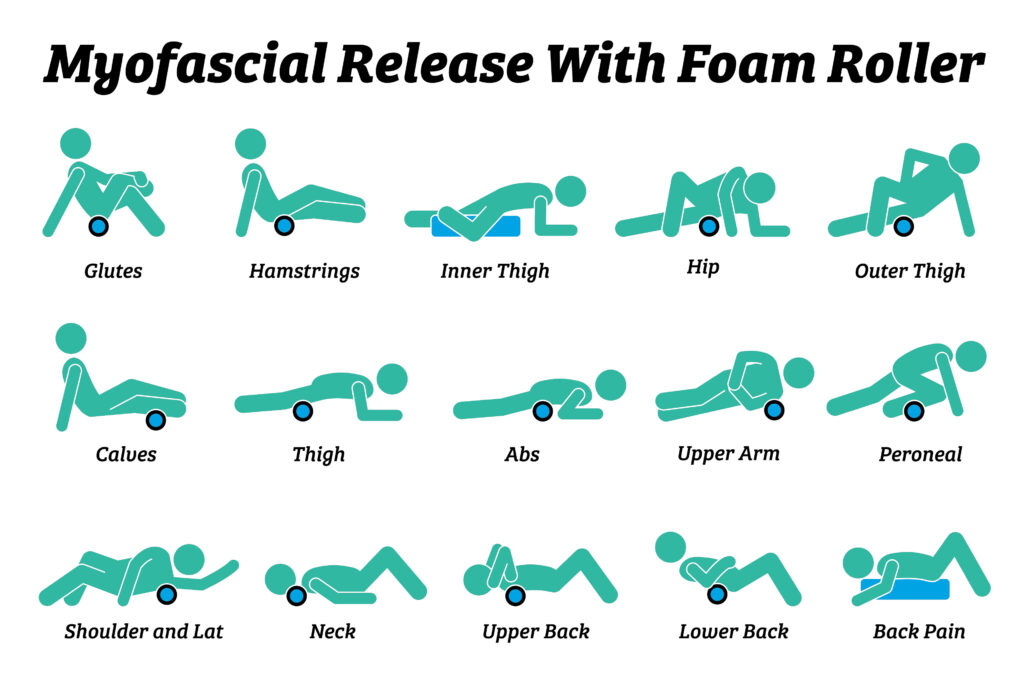
Home Program:
The therapist provides instructions and recommendations for self-care and home exercises to complement the myofascial release therapy. This may include specific stretches, self-massage techniques, or other strategies that the individual can perform between therapy sessions.
Progress Monitoring and Adjustment:
The therapist regularly monitors the individual’s progress, assesses changes in tissue mobility, pain levels, and overall response to treatment. The treatment plan is adjusted based on the individual’s needs, goals, and response to therapy.
Retrograde edema massage is a specialized technique used in occupational therapy to address edema (swelling) in a limb or affected area. It involves manually manipulating the tissues to facilitate lymphatic drainage and reduce swelling. The steps involved may vary depending on the specific technique being used and the individual’s condition:
Assessment:
The occupational therapist performs an assessment to evaluate the individual’s condition, identify the presence of edema, and determine the appropriateness of retrograde edema massage. This assessment includes evaluating the severity and extent of the edema, identifying any contraindications or precautions, and considering the individual’s medical history.
Positioning:
The therapist positions the individual in a comfortable and accessible position that allows for easy access to the affected limb or area. The limb may be elevated to help facilitate lymphatic drainage.
Warm-up:
The therapist may use various methods to warm up the tissues before starting the manual therapy. This can include applying heat packs, using warm towels, or performing gentle exercises or movements to increase blood flow and relax the muscles.
Manual Strokes:
The therapist uses specific manual strokes and techniques to facilitate retrograde edema massage. These strokes typically involve gentle, rhythmic, and repetitive movements that follow the natural direction of lymphatic flow.
Proximal to Distal Sequence:
Retrograde edema massage usually begins proximally, closer to the trunk or body, and progresses distally toward the affected limb. This helps guide the fluid toward the lymphatic drainage pathways and reduces the risk of congestion.
Pressure and Rhythm:
The therapist applies gentle, consistent pressure during the massage, avoiding excessive force that could cause discomfort or damage. The pressure is typically directed toward the trunk or body to encourage lymphatic flow.
Clearing Areas of Lymph Nodes:
The therapist may focus on specific areas where lymph nodes are located, such as the groin, armpit, or neck. Gentle strokes are applied in these regions to facilitate lymphatic drainage from the affected area.
Communication and Feedback:
Throughout the session, the therapist maintains open communication with the individual to ensure their comfort and to gather feedback on the level of pressure, discomfort, or any sensations experienced. This helps guide the therapist in adjusting their techniques and ensuring the individual’s needs are met.
Home Program:
The therapist provides instructions and recommendations for self-care and home management of edema. This may include techniques for self-massage, elevation, exercises, or the use of compression garments to aid in lymphatic drainage and manage swelling between therapy sessions.
Progress Monitoring and Adjustment:
The therapist regularly monitors the individual’s progress, assesses changes in swelling, pain levels, and overall tissue response. The treatment plan is adjusted based on the individual’s needs, goals, and response to therapy.

Cupping therapy is a manual therapy technique used in occupational therapy to promote circulation, relieve muscle tension, and reduce pain. It involves the use of special cups that create suction on the skin, drawing the underlying tissues upward. The steps involved may vary depending on the specific technique being used and the individual’s condition:
Assessment:
The occupational therapist performs an assessment to evaluate the individual’s condition, identify areas of muscle tension or pain, and determine the appropriateness of cupping therapy. This assessment includes evaluating range of motion, muscle tone, identifying any contraindications or precautions, and considering the individual’s medical history.
Positioning:
The therapist positions the individual in a comfortable and accessible position that allows for easy access to the areas being treated. The individual’s skin should be clean and free from lotions or oils that may interfere with the suction of the cups.
Cup Selection:
The therapist selects the appropriate cups for the individual’s needs. Cupping therapy can be done with various types of cups, including glass cups or silicone cups. Glass cups are often used in traditional cupping therapy, whereas silicone cups provide a more controlled and adjustable suction.
Lubrication:
The therapist may apply a small amount of lubricant, such as oil or lotion, to the skin in the areas where the cups will be applied. This helps create a seal and allows the cups to glide smoothly over the skin.
Cup Placement:
The therapist places the cups on the selected areas of the body that require treatment. The cups are usually placed in a way that covers the target muscles or areas of tension. Multiple cups may be used depending on the individual’s needs and the size of the treatment area.
Suction Creation:
The therapist creates suction in the cups using various methods. For glass cups, a flame is briefly introduced to create a vacuum as the heated air cools down inside the cup. For silicone cups, a manual or pneumatic pump is used to create suction.
Cup Application:
The cups are gently placed on the skin, creating a suction effect that draws the underlying tissues upward. The therapist ensures that the cups are secure and comfortable for the individual. The cups may be left stationary or moved along the muscles in a gliding or circular motion.
Duration:
The therapist monitors the individual’s response and determines the appropriate duration for cupping therapy. This can vary depending on the individual’s tolerance, the treatment goals, and the specific technique being used. Cupping therapy sessions typically last between 5 to 15 minutes.
Sensations and Feedback:
Throughout the session, the therapist communicates with the individual to assess their comfort level and gather feedback on the sensations experienced during the cupping therapy. This helps guide the therapist in adjusting the suction intensity, duration, or technique as needed.
Cup Removal:
After the desired duration, the therapist gently removes the cups from the skin. Care is taken to release the suction and minimize any discomfort. The therapist may apply gentle massage or manual techniques to further release tension in the treated areas.

Skilled manual therapy techniques for joint mobilization in occupational therapy are used to improve joint mobility, restore normal joint mechanics, and reduce pain. The steps involved may vary depending on the specific technique being used and the individual’s condition:
Assessment:
The occupational therapist performs an assessment to evaluate the individual’s condition, identify joint restrictions or dysfunctions, and determine the appropriateness of joint mobilization techniques. This assessment may include evaluating joint range of motion, muscle strength, identifying any contraindications or precautions, and considering the individual’s medical history.
Positioning:
The therapist positions the individual and the joint being treated in a comfortable and accessible position that allows for optimal access to the joint. This may involve adjusting the individual’s body position, using pillows, bolsters, or specialized equipment to achieve the desired alignment.
Warm-up:
The therapist may use various methods to warm up the joint and surrounding tissues before starting the manual therapy techniques. This can include applying heat packs, using warm towels, or performing a gentle range of motion exercises to increase blood flow and relax the muscles.
Stabilization:
The therapist provides appropriate stabilization to ensure the joint is supported and secure during the mobilization. This may involve using their hands, belts, or straps to stabilize the joint or adjacent body parts to isolate the movement to the target joint.
Joint Assessment:
The therapist assesses the specific joint motion and identifies any restrictions, limitations, or abnormal movement patterns. They palpate the joint and surrounding structures to gather information about the joint’s condition and guide the selection of appropriate mobilization techniques.
Mobilization Techniques:
The therapist applies skilled and controlled forces to the joint to improve joint mobility and reduce restrictions. These techniques can include gliding, traction, compression, or accessory movements, depending on the joint and the desired therapeutic effect.
Graded Progression:
The therapist progresses the mobilization techniques based on the individual’s response and tolerance. They may gradually increase the amplitude or force of the mobilization, always considering the individual’s comfort and safety.
Communication and Feedback:
Throughout the session, the therapist maintains open communication with the individual to ensure their comfort and to gather feedback on the sensations experienced during the joint mobilization. This helps guide the therapist in adjusting their techniques and ensuring the individual’s needs are met.
Treatment Progression and Duration:
The therapist monitors the individual’s response to the joint mobilization techniques, assessing changes in joint mobility, pain levels, and overall tissue response. This helps guide the treatment progression and determines the appropriate duration for each session.
Home Program and Follow-up:
The therapist provides instructions and recommendations for self-care and home exercises to complement the joint mobilization techniques. This may include guidance on performing specific exercises, stretches, or activities to maintain and enhance the benefits of the joint mobilization between therapy sessions.

The steps involved may vary depending on the specific technique being used and the individual’s condition:
Assessment:
The occupational therapist performs an assessment to evaluate the individual’s condition, identify areas of stiffness, and determine the appropriate manual therapy techniques. This assessment may include range of motion testing, strength evaluation, observation of movement patterns, and gathering relevant medical history.
Warm-up:
The therapist may use various methods to warm up the tissues and increase blood flow before initiating the manual therapy techniques. This can include applying heat packs, using warm towels, or performing gentle exercises or movements to warm up the muscles and joints.
Positioning:
The therapist positions the individual in a comfortable and accessible position that allows for easy access to the affected areas. This may involve sitting, lying down, or assuming specific postures based on the joints being treated.
Soft Tissue Mobilization:
The therapist uses specific techniques such as massage, kneading, or stretching to address muscle tightness and restrictions in the surrounding soft tissues. This helps to improve tissue extensibility and reduce stiffness.
Joint Mobilization:
The therapist applies skilled and controlled forces to the joints to improve joint mobility and reduce stiffness. Techniques such as gliding, traction, compression, or accessory movements may be used, depending on the joints being treated and the individual’s needs.
Range of Motion Exercises:
The therapist guides the individual through active or assisted range of motion exercises to improve joint mobility and flexibility. These exercises may involve gentle stretching, controlled movements, or functional activities targeting the affected joints.
Strengthening Exercises:
The therapist incorporates specific exercises to address muscle weakness and promote stability around the affected joints. These exercises may target specific muscle groups to improve strength and endurance, reducing joint stiffness.
Neuromuscular Re-education:
The therapist utilizes techniques to improve coordination, proprioception, and motor control. This helps the individual regain normal movement patterns and enhance functional activities.
Education and Home Program:
The therapist provides instructions and recommendations for self-care and home exercises to complement the manual therapy techniques. This may include guidance on maintaining joint mobility, applying heat or cold therapy, performing specific exercises, or implementing ergonomic principles.
Progress Monitoring and Adjustments:
The therapist regularly monitors the individual’s progress, assesses changes in joint mobility, pain levels, and overall function. The treatment plan is adjusted based on the individual’s needs, goals, and response to therapy.
Phone:
734.542.9770
586.439.6243
586.439.6310
Standard Hours:
Mon. – Fri.
7:00 am – 7:00 pm
Shelby Township:
Mon – Fri.
9:00 am – 7:00 pm

